The loss of circulating oestrogen can have profound effects on several different systems in the body. It is important to note that not all symptoms around this stage of life are due to loss of hormones and that some may reflect the normal ageing process.
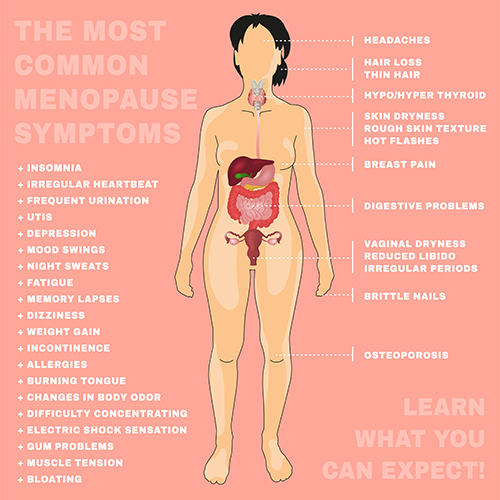
Vasomotor symptoms:
Vasomotor symptoms refer to hot flushes and night sweats. They are very common during the perimenopause and menopause and affect 60-80% of women. Vasomotor symptoms usually decrease with time after the menopause. It is not known exactly why changes in hormone levels bring on vasomotor symptoms. One theory is that it may be related to effects on the brain’s temperature regulatory centre. Oestrogen may also control body temperature by helping blood vessels to dilate to allow heat to be lost through the skin. Obesity, smoking and a history of depression or anxiety all increase the risk of developing vasomotor symptoms.

Skin and hair changes:
Thinning, dryness, loss of elasticity and wrinkling of the skin often occur. Some women develop the sensation of “crawling” under the skin. Wrinkling is made worse by smoking and sun exposure.
Women may notice increased facial hair and thinning of scalp and pubic hair.

Joints and bones:
Some of the commonest symptoms during the menopause are aches and pains in joints and muscle.
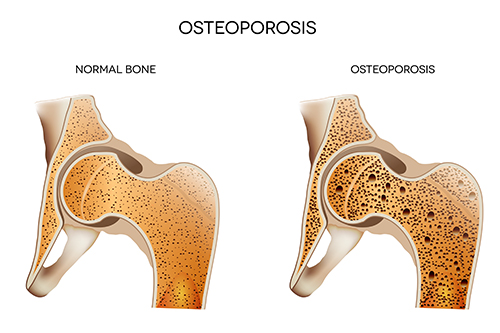
Oestrogen is required for maintaining bone strength and bone mass. One of the most important changes after the menopause is thinning of the bone that could lead to fragile bones (known as osteoporosis). Women lose up to 10% of their bone mass in the first 5 years after the menopause. This bone loss increases the risk of fractures. A fracture is often the first sign that osteoporosis has developed.
Weight changes:
Women naturally gain around half a kilogram per year between the ages of 45 to 55. This weight gain is not because of the menopause. However, reduced hormone levels may cause weight to be distributed differently, leading to increased accumulation of fat in the abdominal region.
Disturbance in mood, memory and sleep:
The occurrence of significant symptoms of depression doubles during the menopausal transition. Feelings of depression and anxiety are thought to be related to swings in the levels of circulating hormones. A previous history of depression, stress and being overweight may increase the risk of mood disturbances during this time.
Problems with sleep affect 35-60% of post-menopausal women. Lack of sleep can exacerbate symptoms of depression and anxiety.
Genitourinary syndrome of the menopause (GSM):
GSM refers to symptoms related to the vulva, vagina, urinary system and sexual function. GSM includes conditions such as vulvovaginal atrophy and atrophic vaginitis. GSM affects around 50% of women after the menopause. GSM often does not develop until at least 2-3 years after the menopause and worsens as women get older. Vaginal symptoms arise because lack of oestrogen leads to thinning of the vaginal lining, reduced blood flow and loss of the supportive connective tissue of the vagina.
GSM can be divided into three main groups of symptoms:
- Vulvovaginal symptoms: Vaginal dryness, burning, vulvar irritation, vaginal discharge, retraction (shrinkage) of the introitus (or external vaginal region) and decreased vaginal elasticity.
- Sexual symptoms: Painful sex (dyspareunia), bleeding with sex, reduced sex drive (loss of libido) and reduced vaginal lubrication.
- Urinary symptoms: Pain when passing urine, passing urine frequently, incontinence and repeated urinary tract infections.
Irregular bleeding:
Irregular bleeding is very common during the peri-menopausal transition before periods stop completely. This is usually the result of changes in hormonal levels. If there is any suspicion about the reason for abnormal bleeding, then an assessment of the lining of the womb is required. This is especially so if bleeding occurs well after menopause.
Transvaginal ultrasound scanning is usually one of the first tests that is performed to evaluate the womb lining (or endometrium). It is used to measure the thickness of the endometrium, which would normally be less than 4mm thick in post-menopausal women. Further investigation such as hysteroscopy or biopsy of the lining is warranted for linings thicker than 4mm. For more information, see my section on Abnormal Uterine Bleeding and Heavy Periods.