Menopause is sometimes referred to as “the change of life” and occurs when levels of the female hormone, oestrogen, become very low. The average age of the menopause is 51 and around one-third of all women in Australia are in the menopausal age-range.
About 80% of menopausal women experience symptoms due to lack of oestrogen, which typically persist for 4-8 years. For 10-20% of women, symptoms persist longer, into their 60s and 70s.
Hormone treatment is very effective for alleviating menopausal symptoms. Recent research shows that hormone therapy has more benefits than risks for most women under 60 and those within the first 10 years of the menopause, especially when delivered via the skin (e.g. patches).
What is menopause?
Menopause reflects the end of ovarian activity which leads to a marked reduction in circulating levels of the hormone, oestrogen.
The average age of the menopause is 51. If menopause occurs between 40 and 45, this is considered an early menopause. If menopause occurs before 40, this is known as premature menopause, also termed premature ovarian insufficiency (POI).
The most obvious sign that ovarian activity has ended is that menstrual periods stop. A woman is said to be post-menopausal if she has not had any periods for 12 months. Stoppage of periods does not happen overnight. The transition occurs gradually over years, usually beginning after age 45. This transitional phase is referred to as the perimenopause. During the perimenopause, periods become more and more irregular and increasingly spread apart, often separated by 2 or more months. Other signs of oestrogen deficiency are also apparent during this time, especially hot flushes and night sweats which are known as vasomotor symptoms.
How is the menopause diagnosed?
The menopause is a normal (physiological) transition that all women experience. Women who begin experiencing menopausal symptoms such as hot flushes above the age of 45 do not require blood tests for making the diagnosis. Blood tests for circulating hormone levels during this time are not very helpful since hormone levels fluctuate widely and may even include spells with very high oestrogen levels.
Blood tests and specialist assessment are important for women whose periods stop before the age of 40.
How does menopause come about?
Ovarian activity reflects the activity of the follicles that make up the ovaries. Each follicle consists of an egg surrounded by an outer covering of cells known as follicular cells. The egg is important for fertility whereas follicular cells produce hormones. Cyclical development of ovarian follicles leads to the release of an egg (ovulation) and to the production of the two female hormones, oestrogen and progesterone. These hormones act on the womb lining causing it to thicken and then to break down, and are therefore responsible for bringing about menstrual bleeding. Females are born with a fixed quota of ovarian follicles (~1-2 million), the numbers of which become less and less throughout life. Eventually, follicle numbers drop to very low levels (less than 1000) leading to a fall in circulating hormone levels, the stoppage of periods, and consequently, the menopause.
The menopause therefore represents the transition into an oestrogen-deficient and infertile state.
For more information on follicles, hormones and ovulation see my sections on The Menstrual Cycle and Ovulation Cycle Tracking and Anovulation and Ovulation Induction.
What are the treatments for menopausal symptoms?
Menopausal hormone therapy:
Menopausal hormone therapy (MHT), formerly known as hormone replacement therapy (HRT), is the best way to control menopausal symptoms such as hot flushes and vaginal dryness and to prevent bone loss.
- MHT can be given either as oestrogen only or as oestrogen and progesterone (known as combined MHT).
- Progesterone is only needed in women who have a uterus. Progesterone prevents the womb lining from undergoing excessive thickening (hyperplasia) as a result of the effects of oestrogen. Women who have had a hysterectomy can use oestrogen on its own and do NOT require progesterone.
- Oestrogens can be given as tablets, skin patches, gels, vaginal creams and vaginal pessaries.
- Progesterone is more difficult to get into the body. Progesterone used for MHT can be given as tablets, patches or vaginal pessaries.
- There are different oestrogen and progesterone preparations. Some have the same chemical structure as those found in the body and are referred to as “body-identical” hormones. Other preparations have a modified chemical structure.
Tibolone (Livial):
Tibolone is a unique hormone that has been engineered to have the combined effects of oestrogen, progesterone and male hormones (or androgens).
Studies show that tibolone is helpful in:
- Reducing hot flushes. Tibolone may not be as effective as MHT in treating hot flushes.
- Reducing bone loss and risk of fractures.
- Improving sexual function.
Tibolone does not increase breast density and does not appear to increase the risk of clots in the veins.
There are some concerns that tibolone may cause an increased risk of cancers of the breast and ovary as well as stroke in women over 60.
Non-hormonal treatments:
The benefits of non-hormonal treatments are mostly restricted to treating hot flushes and night sweats.
- Serotonin-Noradrenaline Reuptake Inhibitors (SNRIs). Examples are Venlafaxine 75-150 mg/day and Desvenlafaxine 100-150 mg/day
- Selective Serotonin Reuptake Inhibitors (SSRIs). Examples are Paroxetine 10-20 mg/day and Escitalopram 10-20 mg/day.
- Gabapentin is used for treating seizures and neuropathic pain. It has a similar structure to the neurotransmitter, gamma-aminobutyric acid (GABA). The starting dose is usually 100 mg three times daily building up to 300 mg three times daily.
- Pregabalin is also similar to GABA. It is used at a dose of 75-150 mg twice daily.
- Clonidine is an alpha adrenergic agonist used for treating hypertension and migraine. The starting dose is 25 mcg twice daily, building up to 50-75 mcg twice daily.
What are the symptoms of the menopause?
The loss of circulating oestrogen can have profound effects on several different systems in the body. It is important to note that not all symptoms around this stage of life are due to loss of hormones and that some may reflect the normal ageing process.
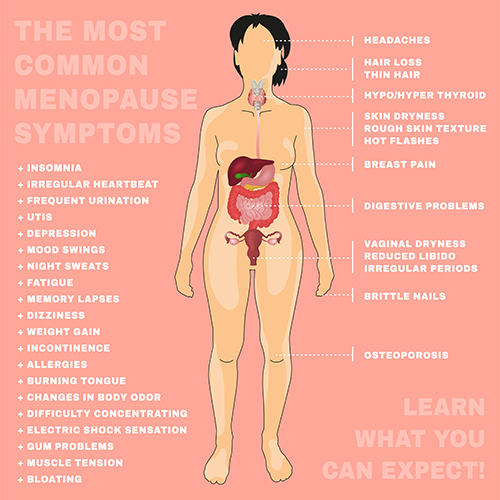
Vasomotor symptoms:
Vasomotor symptoms refer to hot flushes and night sweats. They are very common during the perimenopause and menopause and affect 60-80% of women. Vasomotor symptoms usually decrease with time after the menopause. It is not known exactly why changes in hormone levels bring on vasomotor symptoms. One theory is that it may be related to effects on the brain’s temperature regulatory centre. Oestrogen may also control body temperature by helping blood vessels to dilate to allow heat to be lost through the skin. Obesity, smoking and a history of depression or anxiety all increase the risk of developing vasomotor symptoms.

Skin and hair changes:
Thinning, dryness, loss of elasticity and wrinkling of the skin often occur. Some women develop the sensation of “crawling” under the skin. Wrinkling is made worse by smoking and sun exposure.
Women may notice increased facial hair and thinning of scalp and pubic hair.

Joints and bones:
Some of the commonest symptoms during the menopause are aches and pains in joints and muscle.
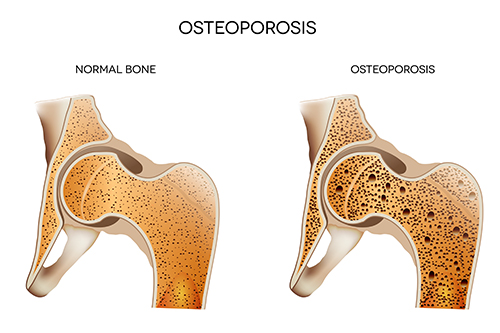
Oestrogen is required for maintaining bone strength and bone mass. One of the most important changes after the menopause is thinning of the bone that could lead to fragile bones (known as osteoporosis). Women lose up to 10% of their bone mass in the first 5 years after the menopause. This bone loss increases the risk of fractures. A fracture is often the first sign that osteoporosis has developed.
Weight changes:
Women naturally gain around half a kilogram per year between the ages of 45 to 55. This weight gain is not because of the menopause. However, reduced hormone levels may cause weight to be distributed differently, leading to increased accumulation of fat in the abdominal region.
Disturbance in mood, memory and sleep:
The occurrence of significant symptoms of depression doubles during the menopausal transition. Feelings of depression and anxiety are thought to be related to swings in the levels of circulating hormones. A previous history of depression, stress and being overweight may increase the risk of mood disturbances during this time.
Problems with sleep affect 35-60% of post-menopausal women. Lack of sleep can exacerbate symptoms of depression and anxiety.
Genitourinary syndrome of the menopause (GSM):
GSM refers to symptoms related to the vulva, vagina, urinary system and sexual function. GSM includes conditions such as vulvovaginal atrophy and atrophic vaginitis. GSM affects around 50% of women after the menopause. GSM often does not develop until at least 2-3 years after the menopause and worsens as women get older. Vaginal symptoms arise because lack of oestrogen leads to thinning of the vaginal lining, reduced blood flow and loss of the supportive connective tissue of the vagina.
GSM can be divided into three main groups of symptoms:
- Vulvovaginal symptoms: Vaginal dryness, burning, vulvar irritation, vaginal discharge, retraction (shrinkage) of the introitus (or external vaginal region) and decreased vaginal elasticity.
- Sexual symptoms: Painful sex (dyspareunia), bleeding with sex, reduced sex drive (loss of libido) and reduced vaginal lubrication.
- Urinary symptoms: Pain when passing urine, passing urine frequently, incontinence and repeated urinary tract infections.
Irregular bleeding:
Irregular bleeding is very common during the peri-menopausal transition before periods stop completely. This is usually the result of changes in hormonal levels. If there is any suspicion about the reason for abnormal bleeding, then an assessment of the lining of the womb is required. This is especially so if bleeding occurs well after menopause.
Transvaginal ultrasound scanning is usually one of the first tests that is performed to evaluate the womb lining (or endometrium). It is used to measure the thickness of the endometrium, which would normally be less than 4mm thick in post-menopausal women. Further investigation such as hysteroscopy or biopsy of the lining is warranted for linings thicker than 4mm. For more information, see my section on Abnormal Uterine Bleeding and Heavy Periods.
What can I do to help with menopausal symptoms?
Lifestyle changes including healthier eating habits, regular exercise and maintaining a healthy weight are beneficial.
It is advisable to avoid triggers for hot flushes such as alcohol, smoking and spicy foods.
Cognitive Behaviour Therapy (CBT) and Clinical Hypnosis may help some women.
Available studies do not find there is any benefit from Yoga, Paced Respiration, Acupuncture, Reflexology, Homeopathy or Chiropractic interventions.
Is hormone treatment risky and does it increase the risk of breast cancer?
The Women’s Health Initiative (WHI) studies from 2002 and 2004 raised alarm bells regarding MHT usage. Importantly, however, subsequent studies, and improved hormonal formulations, have provided a far better understanding of the risks of MHT. These new studies show that MHT provides more benefits than risks when used within the first 10 years of the menopause and in women under 60.
Some key facts related to MHT:
- MHT does not increase the risk of breast cancer if used for less than 5 years. There may be a small increase (about 1 extra case per 1000 women) in breast cancer when using combined MHT (oestrogen + progesterone) in tablet form for longer than 5 years.
- The risk of breast cancer does not appear to be increased if certain types of progesterone are used, like Dydrogesterone and those with an identical structure to the body’s own progesterone (e.g. Prometrium).
- There is no increased risk of breast cancer for oestrogen-only MHT.
- Based on the above 3 points, any increased risk for breast cancer related to MHT appears to be due to progesterone usage and not oestrogen.
- MHT does not increase the number of heart attacks or death from heart disease if taken within 10 years of the menopause. Indeed, oestrogen-only MHT may decrease the risk of heart disease.
- In women less than 60, MHT used in tablet (oral) form causes a very small increased chance of having a blood clot. This occurs because hormones taken via the mouth pass through the liver after being absorbed by the gut and cause a change in the production of clotting factors in the liver. The absolute risk of having a clot due to MHT remains very small, 1 extra case for every 1000 women on MHT.
- MHT given via the skin (e.g. patches) bypasses the liver and has not been found to increase clot formation. This is the preferred form of MHT for women with increased risk for clots (e.g. overweight women and smokers). A very large study involving over 450,000 women in the UK was published earlier this year in the British Medical Journal and confirmed that using oestrogen via the skin (e.g. patches and gel) does not increase the risk of blood clots.
- The risk of blood clots is higher for combination MHT than for oestrogen-only MHT.
- MHT does not increase the risk of stroke in women under 60 or within the first 10 years of the menopause who do not have risk factors for stroke.
- MHT is not advisable for women who have had hormone-dependent cancers such as cancers of the breast and womb lining (endometrium).
- Vaginal oestrogen is the preferred and most effective treatment for GSM symptoms such as vaginal dryness and burning and painful sexual intercourse. A very recent study based on the large US Nurses’ Health Study found that vaginal oestrogen is very safe and does not increase risks for heart attacks, blood clots, strokes or cancers of the womb and breast.
The risks associated with MHT depend on various factors. The key ones are:
- Age and length of treatment. The safest time is within the first 10 years after menopause and for women under 60.
- Other co-existing conditions. Risks are increased in women who are obese, who smoke and who have had other medical conditions such as clots in the veins or an inherited tendency to form clots.
- Whether progesterone treatment is also required. Some risks associated with MHT (e.g. breast cancer, heart disease and clots in the veins) are more strongly related to the progesterone component.
- Risks associated with progesterone may be minimised by:
- Using body-identical progesterone (see below)
- Delivering progesterone directly to the womb lining instead of through the blood by means of a progesterone-releasing device placed inside the womb (Mirena)
- Using a type of medication called a Selective Estrogen Receptor Modulator (SERM) instead of progesterone to protect the womb lining from oestrogen. One preparation known as DuaviveTM contains the SERM, Bazedoxifene, in combination with conjugated oestrogen.
- The method of administering MHT. Treatments given via the skin (e.g. patches) or the vagina are not associated with the increased risk of clot formation seen with MHT in tablet form. As mentioned above, earlier this year, a very large UK-based study confirmed that oestrogen given via the skin does not increase the formation of blood clots. A very recent study conducted in the USA found that vaginal oestrogen was very safe and did not increase risks for heart attacks, blood clots, strokes or cancers of the womb and breast.
- The structure of the hormones used. Some hormones are identical in structure to those found in the body. These hormones are known as body-identical. Body-identical hormones may be safer than other types of hormones that have different structures.
- Body-identical oestrogen (e.g. 17β-Oestradiol) is available as tablets, patches, gels and vaginal treatments. A recent large study conducted in the UK found that oestrogen in the form of oestradiol is less risky in terms of clot formation compared with conjugated equine oestrogen.
- Body-identical progesterone is available as capsules (Prometrium) that can be used orally or vaginally.
How can I reduce bone thinning during the menopause and treat osteoporosis?
The following are important for maintaining healthy bones:
- Calcium is the key mineral in bone. 1000-1300mg per day is required and can be obtained from the diet. However, up to 60% of postmenopausal women do not meet dietary calcium requirements.
- Vitamin D. Vitamin D is required for calcium to be effectively used in bone formation. Adequate vitamin D levels can be derived from sufficient exposure to sunlight (5-15 minutes of exposure per day). In Australia, 30-50% of postmenopausal women are deficient in vitamin D.
- Physical activity. Weight-bearing exercise such as walking, jogging and dancing help stimulate bone growth.
- Avoidance of smoking and reducing caffeine intake.
Treatments for preventing bone loss and strengthening bone include:
- Combined calcium and vitamin D supplements. This may be necessary if dietary intake is inadequate.
- MHT can increase bone density by about 5% after 2 years and reduces the risk of spinal and hip fractures by approximately 40%.
- Tibolone (see above section “What are the treatments for menopausal symptoms?”)
- Selective Estrogen Receptor Modulators (SERMs). These drugs (e.g. Raloxifene) act like oestrogen on bone leading to an increase in bone mass and reduced fractures. Unlike oestrogen, raloxifene does not stimulate the womb lining. Raloxifene may block oestrogen effects at other sites and so may cause hot flushes.
- Bisphosphonates. These drugs (e.g. Alendronate [Fosamax]) reduce bone loss and fractures.
- Denosumab (Prolia). This also reduces bone loss and fractures.
- Teriparatide (Forteo). This is the bioactive fragment of the hormone known as parathyroid hormone. It increases calcium absorption and bone formation. It may need to be used in conjunction with calcium and vitamin D supplements.
How can I treat vaginal symptoms?
For some women, vaginal symptoms such as dryness, itchiness and painful intercourse are the most bothersome. The options available include:
- General measures: Use of cotton underwear, avoiding tight-fitting underwear, use of low-allergenic washing products, avoidance of scented pads and tampons, use of plain water and avoiding soap for washing the genital area and stopping smoking.
- Dilute bicarbonate of soda washes (half teaspoon of bicarbonate of soda in 1 litre of water).
- Vitamin E may be beneficial
- Non-hormonal vaginal moisturisers (e.g. Replens®)
- Water or silicone-based lubricants for sexual activity
- Vaginal oestrogen (pessaries or creams e.g. Ovestin and Vagifem). It is not necessary to use progesterone if vaginal oestrogen alone is being used.
- If vaginal symptoms do not improve with systemic use of MHT (i.e. in tablet and patch form), adding vaginal oestrogen is often effective.
- Ospemifene. This belongs to the groups of drugs known as Selective Estrogen Receptor Modulators (SERMs).
Is vaginal laser therapy safe for treating vaginal symptoms?
In July 2018, the US Food and Drug Administration (FDA) issued a consumer warning about the use of carbon dioxide (CO2) laser therapy for vaginal cosmetic procedures or ‘vaginal rejuvenation’. The FDA stated that “These products have serious risks and don’t have adequate evidence to support their use for these purposes. We are deeply concerned women are being harmed.”
The first randomised clinical trial involving vaginal laser for treating menopausal vaginal symptoms was published last year (2018). The study reported some benefits with laser treatment. But concerns were raised regarding increased vaginal pain in the group of women using laser treatment.
More extensive clinical research is required before it is known whether laser is safe and effective for treating menopausal vaginal symptoms.
Are complementary, herbal, alternative and other therapies effective for vasomotor symptoms and are they safer than MHT?
There are a wide range of agents in this group including Black Cohosh, Phytoestrogens (including Red clover), Wild Yam Cream, Evening Primrose Oil, Flaxseed, Ginseng, Maca, Pine Bark (Pycnogenol), Pollen extract, Siberian Rhubarb, Vitamin E, Omega-3, Magnesium and Homeopathy.
Treatment with most of these agents has not been tested in high-quality clinical trials. In most cases, there is no clear evidence that vasomotor symptoms are improved. There is also uncertainty surrounding safety and dosing.
Are compounded bioidentical hormone preparations safer than MHT?
MHT refers to the use of pharmaceutical-grade hormones that have been extensively validated in clinical trials.
Unlike MHT, hormone preparations compounded in pharmacies in the form of creams, troches and pessaries – often referred to as “bioidentical” hormones – have not been subjected to rigorous evaluation of efficacy or safety.
One of the concerns with compounded preparations is that the progesterone component may not reliably protect the womb lining from oestrogen action. There have been cases of cancer of the womb lining in women using compounded bioidentical hormone treatments. There are also concerns regarding potential contamination with impurities that could have serious consequences.
The Australasian Menopause Society does NOT recommend the use of compounded bio-identical hormones in any form.
Can an AMH blood test predict when I will undergo menopause?
AMH stands for Anti-Müllerian Hormone. AMH is produced by a particular group of follicles in the ovary. Since ovarian follicle numbers decline with age, AMH levels also decline with age.
Studies have investigated whether a woman’s AMH level can predict when she might enter menopause. These studies have produced contradictory results. At present, it is unclear whether AMH is useful for predicting menopause onset. This year, the American College of Obstetricians & Gynaecologists (ACOG) concluded that “the use of antimüllerian hormone as a predictor of the onset of the menopause is unsuitable for clinical practice at this time”.
For more information on AMH, see my section on “AMH, Ovarian Reserve and the Egg Timer Test”.
Who should I see for advice on the menopause?
More and more research into the menopause is emerging. The results from these studies are constantly changing the landscape of treatments for the menopause.
Regarding MHT, the pendulum has swung back towards promoting usage as increasing evidence of safety accumulates. Advice on MHT is also being influenced by the emergence of newer and safer hormonal formulations and increasing evidence for the safety of using hormones via routes such as skin and vagina.
If you have concerns about the menopause, it is very important to see a specialist who is fully up-to-date with the latest information and evidence regarding menopause management, and who is able to evaluate your individual circumstances in order to devise the safest and most effective regime suited to you. Prof Homer is a Sub-specialist in Reproductive Endocrinology with both the Australian and the British Royal Colleges and has extensive expertise in ovarian biology, hormones and management of the menopause.