PCOS Doctor Brisbane
PCOS is a common condition estimated to affect 8-13% of women of reproductive age, with up to 70% of affected women remaining undiagnosed. International guidelines for the assessment and management of PCOS have recently been released in 2018.
What are the symptoms of PCOS?
Women with PCOS can experience a variety of symptoms, such as irregular or absent periods, infertility, excess body hair growth, acne and metabolic disturbances that lead to an increased risk of developing diabetes and cardiovascular problems.
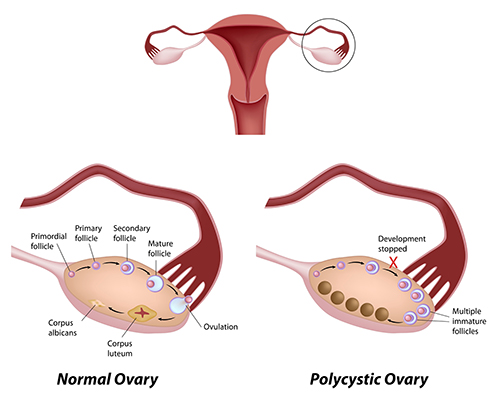
What are polycystic ovaries?
Polycystic ovaries (PCO) are ovaries that have a “polycystic” appearance. PCO is not the same as PCOS. The term polycystic is a misnomer since so-called polycystic ovaries do not contain typical cysts, which in Gynaecology usually refers to a cystic swelling at least 5 cm in diameter. Polycystic ovaries refer to the presence on ultrasound scan of multiple immature follicles measuring 2-9 mm (less than 1 cm) in diameter.
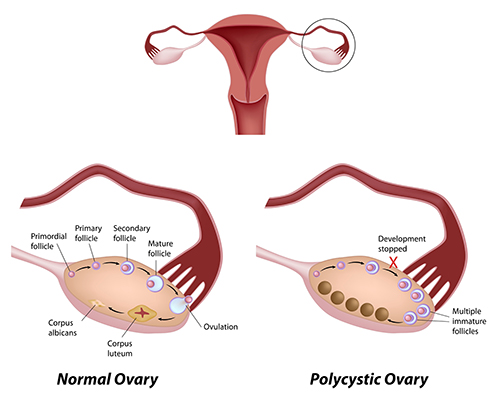
What are ovarian follicles?
Follicles are the functional units of the ovary. Each follicle is comprised of an egg surrounded by follicular cells. In addition to producing the eggs required for fertility, ovarian follicles are also responsible for producing the female hormones, oestrogen and progesterone. Over the course of 2-3 months, the earliest follicle-stage known as the primordial follicle, develops into a mature follicle, leading to the release of a mature egg at ovulation. In the case of PCOS, follicle development becomes arrested at an immature stage and no eggs are released resulting in infertility.
How are PCO and PCOS diagnosed?
The “cysts” in PCO are actually small immature follicles, which, as explained above, are normal features of all ovaries; when large numbers of antral follicles are visible on ultrasound scan (>20 in the most recent guidelines released in 2018) and/or the volume of the ovary is increased, the ovary is considered to be polycystic.
For a diagnosis of PCOS, two out of three of the following criteria need to be present:
- Polycystic appearing ovaries (PCO) on ultrasound.
- Irregular, infrequent or absent periods, which reflect infrequent or absent ovulation (ovulation is the release of an egg from the ovary).
- Increased levels of male hormones or signs of increased male hormone effects, such as excessive body hair growth.
How is PCOS treated?
It is important to stress that the incidental discovery of polycystic-appearing ovaries on ultrasound scan, when present on its own, does not require treatment.
For PCOS, treatment should be targeted at the main problem, but should also consider the bigger picture of longer-term overall health. Some of the problems that women with PCOS experience include menstrual cycle irregularity, signs of male hormone excess and infertility.
Lifestyle modification:
For overweight PCOS patients, healthy eating and regular physical activity to lose weight are very important, and may be combined with the use of metformin. A healthy lifestyle not only helps to improve menstrual cycle regularity and fertility, it also reduces the risks of medical conditions that women with PCOS are prone to later in life such as diabetes.
Hormonal medication:
The combined oral contraceptive pill can be used to help regularise periods and has beneficial effects when signs of male hormone excess (e.g. excess hair growth) are present. Because cycle irregularity in PCOS is due to problems with ovulation, women undergoing ovulation induction treatment for fertility reasons (see below) will also experience improved cycle regularity.
It is important that women with PCOS not go for more that 3 months without having a period since this risks the lining of the womb (or endometrium) getting too thick.
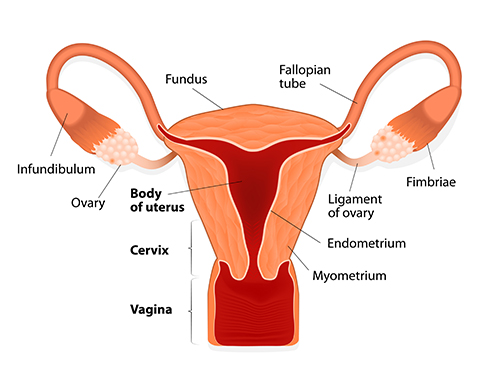
Women with PCOS have an increased risk of developing excessive thickening of the womb lining (known as endometrial hyperplasia), which leads in turn to a 2- to 6-fold increased risk of developing cancer of the womb.
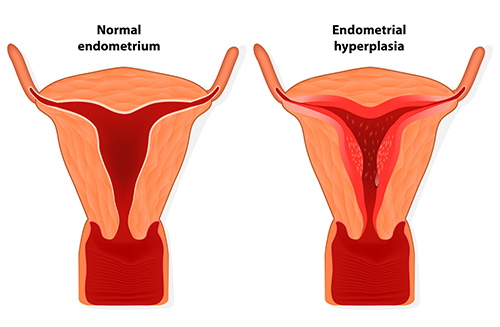
Excessive thickening of the womb lining can be prevented by artificially inducing a period using a 7-10 day course of progesterone tablets at least once every 3 months.
Ovulation induction for infertility:
Because women with PCOS often do no release an egg (ovulate), many will experience infertility. If other factors that determine a couple’s fertility are normal (e.g. sperm quality), then the use of medication to cause the release of an egg (ovulation induction) is an effective treatment. Oral medications used for ovulation induction include letrozole, clomiphene citrate and metformin. In difficult cases, hormonal injections and laparoscopic surgery for “drilling” polycystic ovaries may be used. Letrozole is currently the recommended first line treatment for ovulation induction in women with PCOS. Ovulation induction should be closely supervised by a trained fertility specialist. In cases in which, ovulation induction is not successful, or there are other co-existing causes for infertility, such as tubal blockage or a significant sperm problem, assisted reproductive treatments (ART) like IVF may be required.
How can I get help for PCOS?
PCOS is a complex medical condition requiring extensive expertise for effective management. Professor Homer has 20 years’ experience in all aspects of PCOS management. He trained and worked at the PCOS clinic at University College London Hospitals, one of Europe’s leading Reproductive Medicine Units. Over the years Hayden has developed extensive expertise in undertaking the appropriate investigations suited to each individual case as well as the full range of treatments for infertility (ovulation induction, IVF etc.) that may be required.