Endometriosis is a frequent cause for pelvic pain and affects around 10% of women or more. Awareness of endometriosis and the severity of symptoms it can cause is increasing. The Australian Federal Government has recently invested $4.5M in the National Action Plan for Endometriosis with the aim of improving understanding, awareness and treatment of the disease.
What is endometriosis?
The lining of the womb is known as the endometrium.
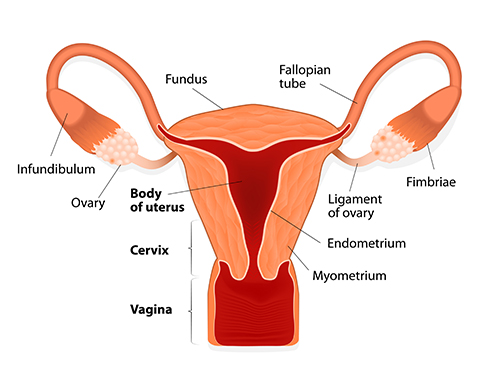
Every month, the endometrium becomes thickened under the influence of oestrogen circulating in the blood. If pregnancy does not occur, the endometrial lining is shed through the neck of the womb (or cervix) and the vagina as the menses.
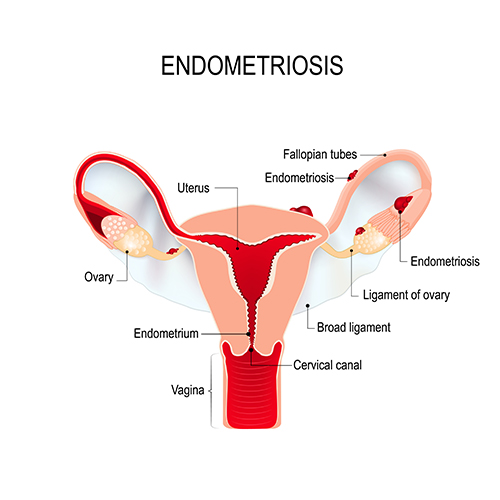
Endometriosis refers to the presence of endometrium outside of its normal location within the cavity of the womb. Endometriosis deposits are most often located in the pelvic cavity, for instance, on the ovaries, on the womb, between the womb and bowel (known as the Pouch of Douglas) and on the surface of the bowel. Deposits can occasionally be located at much more distant sites such as the lung.
How common is endometriosis and how is it diagnosed?
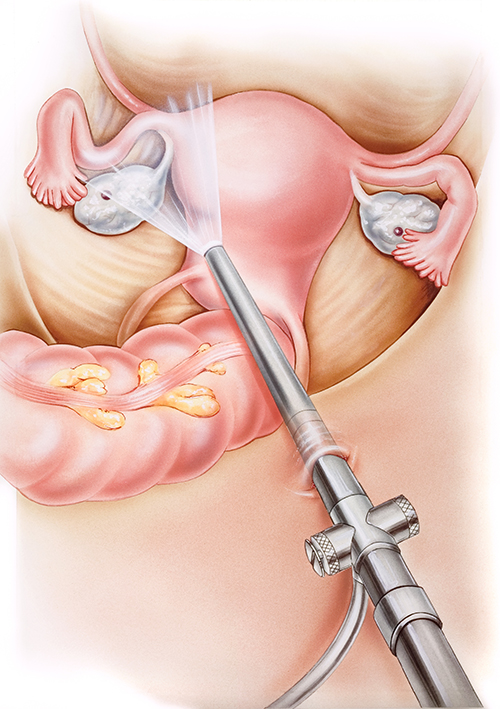
Diagnosing endometriosis may not be straightforward and there is no specific blood test that can be done. Some forms of endometriosis such as endometriotic cysts on the ovaries (known as endometriomas or “chocolate” cysts) can be identified using ultrasound scan and with other imaging tests like MRI. However, small deposits in the pelvis will not be detectable using these tests. Keyhole surgery (laparoscopy) is the gold-standard method for diagnosing endometriosis as it allows direct visualisation of the pelvic cavity.
Because there is no simple test for diagnosing the condition, it is difficult to know for certain how common endometriosis is. Estimates suggest that it may affect up to 10% of women.
What are the symptoms of endometriosis?
Endometriosis can be a crippling condition. The main symptom is lower abdominal and pelvic pain.

Pain can take different forms, including chronic pelvic pain (pain lasting >6 months), severe pain associated with menses (termed dysmenorrhoea), pain associated with sexual intercourse (dyspareunia) and painful bowel motions.
Endometriosis is also associated with infertility.
Why does endometriosis cause pain?
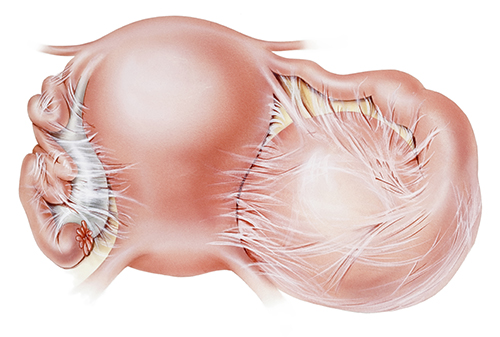
Endometriotic deposits in the pelvis and other abnormal sites undergo changes like the normally sited endometrium within the womb; ectopic deposits thicken and then breakdown on a cyclical basis in synchrony with the womb lining. Unlike the womb lining, however, blood from deposits outside the womb have no path for getting out of the body and accumulate within the pelvic cavity. These bleeding sites also trigger a local inflammatory response. All these changes cause pain. Because these events that cause pain occur in relation to the menstrual cycle, pain with endometriosis is often cyclical and may intensify at the time of the menses. Pain can also come about from the scarring (known as adhesions) caused by repeated episodes of bleeding from these endometriosis sites that cause the pelvic organs to become stuck to one another.
Does endometriosis cause infertility?
There is a strong association between endometriosis and infertility. Endometriosis is commonly seen in women having problems conceiving. Advanced forms of endometriosis, for instance, those with chocolate cysts in the ovaries, or severe scarring that damages the Fallopian tubes, can reduce the chances of conceiving. Less severe forms of endometriosis are also associated with infertility, perhaps due to inflammatory changes with the pelvic cavity that cause harm to sperm, eggs or embryos.
There is evidence that treating milder forms of endometriosis using key-hole surgery improves natural fertility. It is unclear whether surgical treatment of endometriosis before IVF improves the chances of IVF success.
What are the treatments for endometriosis?
The UK National Institute for Health and Care Excellence (NICE) issued guidelines for managing endometriosis in 2017. Treatment can be with oral medication or with surgery and depends on the primary symptoms and importantly, the patient’s desire for pregnancy. For managing pain, simple pain-killers can be effective and are often used as a first-line option. Since endometriosis is hormone-dependent, other treatment options include hormonal manipulation, for instance, with the combined oral contraceptive pill. A new drug recently approved by the US FDA known as Elagolix (marketed as Orilissa), shows promise in treating endometriosis symptoms. The surgical option involves laparoscopic surgery, which can confirm the diagnosis, map the extent of the disease and allow deposits and chocolate cysts to be cut away.
How can I get help with endometriosis?
Women with suspected endometriosis require expert and patient work-up, as well as highly individualised management planning, carefully considering their desire for fertility.
Professor Homer has extensive experience in diagnosing and treating endometriosis as well as undertaking fertility treatment in cases complicated by endometriosis. He worked at the Endometriosis Unit at University College London Hospital (UCLH), a central referral specialist unit for complex endometriosis housing one of the UK’s largest laparoscopic surgical units.
He undertook advanced laparoscopic surgical training and practised for several years as a Laparoscopic Surgeon at UCLH.