Abnormal uterine bleeding (or AUB), which includes heavy periods, is a common condition affecting 14-25% of women of reproductive age. AUB has significant effects on a woman’s physical, emotional, social and mental quality of life.
What is abnormal uterine bleeding and heavy menstrual bleeding?
Abnormal uterine bleeding (or AUB) refers to any bleeding from the womb that is abnormal in amount, regularity or timing and that has been present for 6 months or more. Heavy periods or heavy menstrual bleeding (HMB), previously referred to as menorrhagia, is one type of abnormal uterine bleeding in which, excessive blood loss interferes with a woman’s quality of life.
What are the causes of abnormal uterine bleeding?
The International Federation of Obstetrics & Gynaecology (FIGO) now recommend that abnormal uterine bleeding be categorised based on the underlying cause using the PALM-COEIN system.
PALM-COEIN stands for:
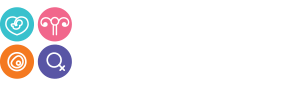
P = Polyps: These are localised thickenings of the lining of the womb. They become increasingly common as women get older.
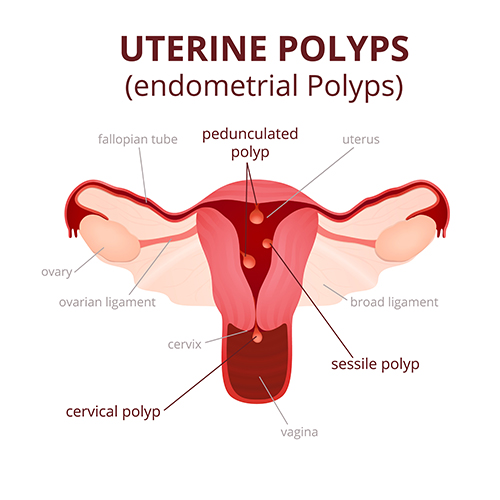
A = Adenomyosis: This refers to the ingrowth of the lining of the womb into the muscle of the womb and usually causes womb enlargement.
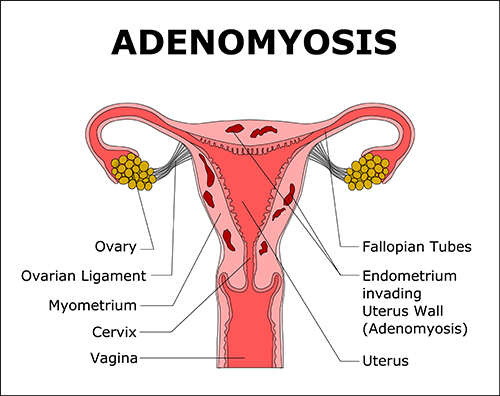
L = Leiomyoma (or Fibroids): Fibroids (or myomas) are the commonest tumours found in women and one of the commonest causes of heavy bleeding. By age 50, almost 70% of white women and more than 80% of black women will have developed at least one fibroid. Fibroids are made up of muscle cells and connective tissue cells and are almost always non-cancerous. There are different types of fibroids depending on their location within the wall of the womb. Those located closest to the lining of the womb (or submucosal fibroids) are thought to be the most problematic regarding bleeding problems. For more information, see my section on Uterine Fibroids.
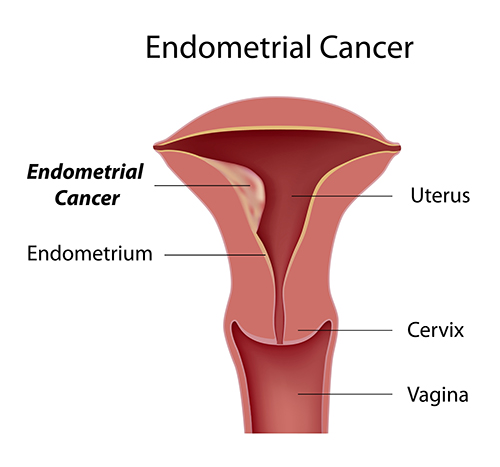
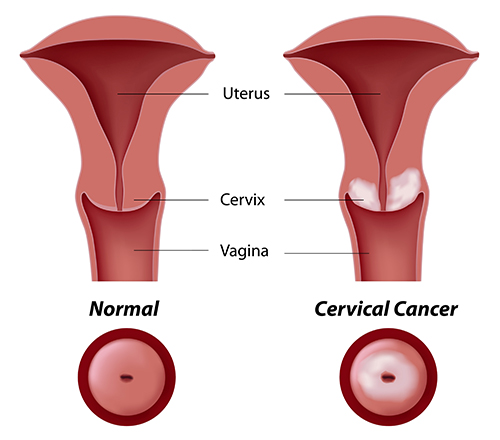
M = Malignancy (or cancer). Cancer of the womb lining or endometrial cancer is the commonest form of gynaecological cancer in the western world. It is very rare in women before the menopause. Obesity and PCOS are associated with an increased risk of developing endometrial cancer. Cancer of the neck of the womb (or cervical cancer) can also cause abnormal bleeding.
C = Coagulopathies. Coagulopathy refers to a tendency to bleed excessively due to defects in the clotting mechanism. Coagulopathies such as Von Willebrand disease are reported to be present in around 13% of women with heavy menstrual bleeding.
O = Ovulatory. This category refers to women who do not ovulate regularly. In these instances, only one hormone, oestrogen, is produced and can cause excessive thickening of the lining of the womb. The combination of anovulation and excessive thickening of the lining of the womb leads to infrequent periods (spaced more than 38 days apart) that are very heavy. One of the commonest causes of anovulation and of this pattern of bleeding is PCOS, although there are other causes such as high prolactin levels. For more information, see my sections on The Menstrual Cycle and Ovulation Tracking; Anovulation and Ovulation Induction, and; PCOS.
E = Endometrial. Women in this category typically present with regular heavy periods and a normal womb structure. Making this diagnosis requires exclusion of other causes such as fibroids or polyps. It is thought to arise due to an imbalance of chemicals such as prostaglandins and clotting factors within the womb lining.
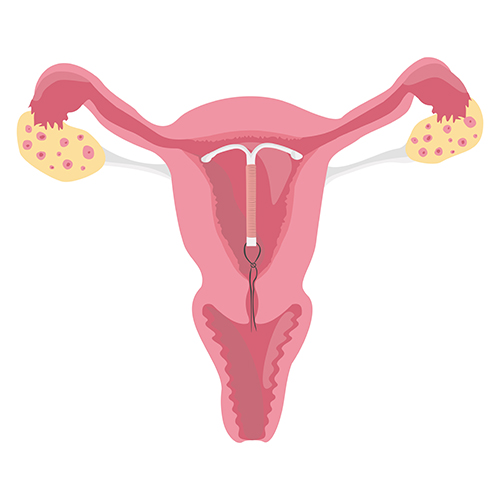
I = Iatrogenic. This refers to abnormal bleeding that is brought about due to another treatment. For instance, an intrauterine device (IUD) can sometimes cause abnormal bleeding by causing inflammatory changes within the womb lining.
N = Not otherwise classified. This is used to refer to very rare conditions or ones that are poorly defined. Examples include aneurysms of blood vessels within the womb or chronic inflammation of the womb lining (endometritis) in the absence of an IUD.
How can I find out which cause of abnormal bleeding I have?
Your history and examination will give a clue as to the cause of your abnormal bleeding. A history of infrequent periods and signs of male hormone excess (such as excess facial hair growth) would point to PCOS with anovulation as the cause. Use of the anticoagulant, warfarin, may cause heavy bleeding. Examination of the pelvis may identify an enlarged womb in cases of adenomyosis or fibroids. Swabs should be obtained to screen for infection. It is important to check that Pap smears are up to date and whether they have been normal.
Ultrasound scanning is an extremely important tool during the workup for abnormal bleeding since it will identify polyps, adenomyosis and fibroids. It will also determine whether the womb lining is excessively thickened.
Obtaining a sample of the lining of the womb (endometrial biopsy) may be indicated if there is a suspicion of cancer. Sampling can be undertaken in the clinic using a fine biopsy tube (known as a Pipelle sampler) or by means of a hysteroscopy.
Blood tests are also important. A full blood count should be done to determine whether there is anaemia or low iron stores as a result of abnormal bleeding. Blood tests will also identify other conditions such as problems with clotting; high male hormone levels as seen in PCOS and high prolactin levels (with hyperprolactinaemia). For more information, see my section on Anovulation and Ovulation Induction.
What treatments are available for abnormal and heavy bleeding?
A very important consideration when deciding on treatment options is a woman’s plans for fertility. If pregnancy is a priority, treatments that remove the womb (hysterectomy) or that block the release of an egg are obviously inappropriate.
There are a range of treatment options available that need to be targeted to the individual circumstances. Treatment should aim to remove the underlying problem wherever possible. Hence, in cases of submucous fibroids and polyps, it is preferable that they be removed using hysteroscopic surgery.
Treatment options include:
- Mefenamic acid: 500 mg three times daily starting 1-2 days before the onset of bleeding.
- Tranexamic acid: 1 gram three or four times daily for up to 4 days
- Combined oral contraceptive pills: Effective in regularising periods. Unsuitable for use in smokers due to increased risk of clot formation.
- Progesterone: Use from Day 5 to Day 26 of cycle. Shorter duration of progesterone usage has not been found to be effective.
- Mirena IUS: This is a progesterone-releasing IUD that is extremely effective in treating heavy menstrual bleeding. It lasts for 5 years after insertion and is also a highly effective form of contraception. It is less effective when the womb cavity is distorted by fibroids.
- Ulipristal acetate (Esmya): Used in cases of uterine fibroids at 5 mg daily from the start of the period for up to 3 months. Caution with use due to recent concerns regarding rare cases of severe liver damage.
- GnRH analogues: These create a temporary menopause by blocking the production of the hormones, FSH and LH. This then blocks oestrogen production causing the lining to become very thin. These drugs can only be used for a few months as the loss of oestrogen may cause thinning of the bones. GnRH analogues are often used to shrink fibroids prior to surgery. See my section on The Menstrual Cycle and Ovulation Tracking for more information.
- Uterine artery embolization (UAE): Caution is advised in women planning pregnancy. Prof Homer’s research found an increased risk of miscarriage after UAE. See my section on Uterine Fibroids for more information.
- Ablation of the womb lining: Using devices such as NovaSure and Thermal Balloons.
- Hysteroscopic surgery to remove the lining of the womb. This is known as Trans-Cervical Resection of the Endometrium (TCRE)
- Hysteroscopic surgery to remove submucous fibroids. This is known as Trans-Cervical Resection of Fibroids (TCRF)
- Hysteroscopic surgery to remove polyps. This is known as Trans-Cervical Resection of Polyps (TCRP)
- Laparoscopic surgery to remove fibroids that may be predominantly located within the muscle layer of the womb (intramural fibroids).
- Hysterectomy: May be performed via laparoscopic surgery in some cases.