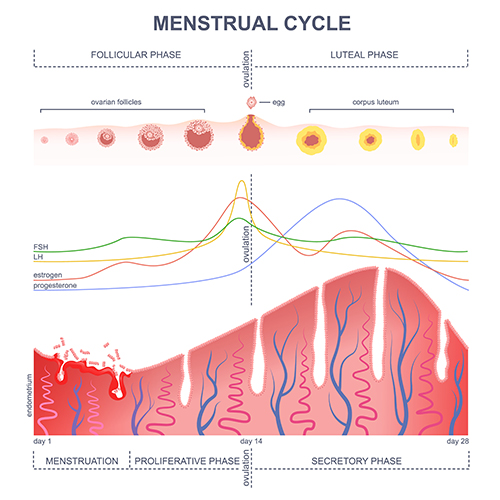
During a normal menstrual cycle an egg is released from the ovary at the time of ovulation. Following release from the ovary, the egg is usually picked up by the Fallopian tube and can survive there for up to 2 days. Understanding how your cycle works and carefully monitoring it can help improve your fertility chances.
How does the menstrual cycle come about?
When is the fertile time of the menstrual cycle?
The fertile time of the cycle coincides with when the egg has been released from the ovary and it is sitting within the end portion of the Fallopian tube. This is usually around 2 weeks before the start of the next menstrual bleed. This means that for a typical 28-day cycle, the fertile time is around 14 days after the bleed started (Day 14). The fertile time will differ depending on cycle length. For instance, for a 32-day cycle, the fertile time is around Day 18. The fertile time, and a couple days either side of it, are the best times for having sexual intercourse in order to optimise the chances of becoming pregnant.
How can I detect when ovulation will occur?
The most accurate way to determine the timing of ovulation is to track ovarian follicle development using ultrasound scanning. In this way, follicle growth can be directly seen with ultrasound and the precise timing of the LH surge determined using blood tests. This is called “cycle tracking” or “ovulation tracking”. Ultrasound scanning also provides other very valuable pieces of information, for instance, about ovarian reserve (the numbers of eggs in the ovary) and whether or not the womb lining is developing properly during the cycle. It will also identify other abnormalities in the womb that might affect pregnancy success such as fibroids and polyps.
Another option is to monitor for the LH surge in the urine. This is how ovulation detector kits work. When LH levels surge in the blood, LH is expected to enter the urine and to be detected using the kit.
The egg is released 1-2 days after the LH surge, so intercourse around the time of the LH surge will increase the chances for sperm to interact with the egg.
How can I get help monitoring my cycle to improve pregnancy chances?
A fertility specialist can help you by monitoring the development of follicles in the ovary and the lining of the womb using ultrasound and blood tests. This will also identify any potential problems that may need to be treated to improve pregnancy chances. Prof Homer has extensive experience with cycle monitoring and optimising fertility prospects.